Oral Health as We Age: A Guide to Dental Care for Seniors
Maintaining oral health in older age is more important than ever. As we grow older, the condition of our teeth, gums, and mouth doesn’t just impact how we eat or speak—it can affect our entire body. At Just Better Care, we’re passionate about supporting seniors with personalised oral care solutions that promote both dental and general health.
This guide will explore the key components of an oral health assessment for seniors, the consequences of neglecting dental hygiene, and practical tips for senior dental care, especially for those with disabilities or chronic conditions.
Why Oral Health is Crucial for Seniors
Good oral hygiene isn’t just about a nice smile—it's about preventing disease. Older adults often face complex oral health challenges due to:
- Long dental histories involving crowns, bridges, implants, or dentures
- Reduced saliva production (dry mouth), a common side effect of medications
- Limited mobility or cognitive decline, making oral hygiene routines harder to follow
- A false belief that tooth loss is inevitable in aging
Preventive dental care for elderly adults can stop problems before they escalate and safeguard their overall health.
What Is an Oral Health Assessment?
An oral health assessment for older adults involves checking the teeth, gums, and mouth for early signs of problems. Here’s what’s typically evaluated during a routine or at-home check:
- Lips – Look for color changes, swelling, chapping, or lumps.
- Tongue – Check for patches, coating, ulcers, or swelling.
- Gums and tissues – Assess for bleeding, color changes, swelling, or loose teeth.
- Saliva – Dry mouth (xerostomia) is common in seniors and can lead to decay and infection.
- Teeth – Look for cracks, cavities, wear, and any bite irregularities.
- Dentures – Ensure they fit properly and aren't causing irritation or ulcers.
- Cleanliness – Is there visible plaque, tartar, staining, or food debris?
- Pain indicators – Seniors may not vocalize pain but may chew on one side or avoid eating.
Developing an Oral Health Care Plan
A comprehensive oral health plan for elderly customers should include:
- Toothbrush type and brushing frequency
- Interdental care tools (floss, interdental brushes)
- Mouth aids (props, disclosing tablets)
- Mouth rinses and toothpaste (sensitive or high-fluoride formulas)
- Dry mouth treatments
- Assistance level – Determine if support is needed for brushing and flossing
- Dental visit schedule – Seniors need regular cleanings and check-ups
Creating a routine with clear instructions can make daily oral hygiene for older adults easier, especially for those with dementia or physical impairments.
Consequences of Poor Oral Health in Seniors
Neglecting oral health in later life can lead to significant health issues. Common dental diseases in elderly people, such as periodontal disease and tooth decay, can affect:
- Nutrition – Difficulty chewing may lead to poor dietary choices.
- Mental health – Missing teeth or bad breath can harm self-esteem.
- Speech – Oral disease may affect speech clarity and confidence.
- Systemic health – Bacteria from gum infections can enter the bloodstream.
Chronic Conditions Linked to Poor Oral Hygiene in Seniors
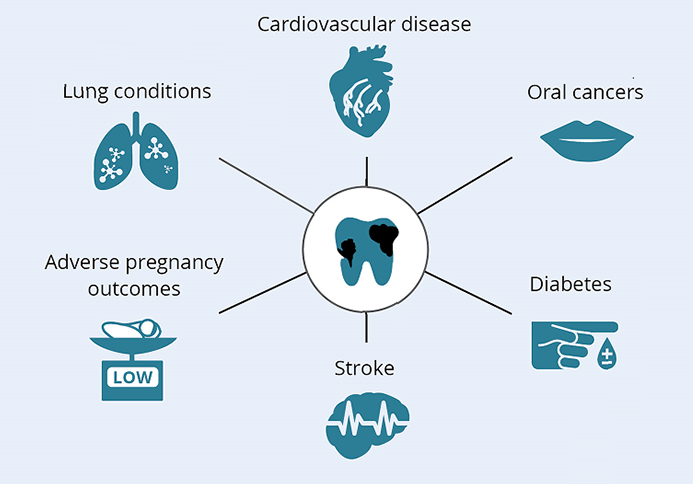 1. Heart Disease and Stroke
1. Heart Disease and Stroke
Studies show a clear connection between gum disease and cardiovascular health. Inflammation from oral infections may contribute to hardened arteries and increase the risk of stroke or heart attack.
2. Diabetes
Poor dental care makes blood sugar harder to control. Likewise, high blood sugar increases the risk of gum infections in diabetics.
3. Lung Infections
Inhaled oral bacteria can lead to pneumonia in elderly patients, especially those in assisted living or with chronic respiratory conditions.
4. Digestive Issues
Oral bacteria can contribute to stomach ulcers, acid reflux, and other gastrointestinal disorders.
5. Inflammatory Bowel Disease (IBD)
Emerging research links gum disease to IBD, including Crohn’s disease and ulcerative colitis, suggesting a shared inflammatory response.
6. Rheumatoid Arthritis
There’s a bidirectional relationship between RA and periodontitis, with inflammation worsening both conditions.
Oral Health and Brain Health in Seniors
There’s growing evidence that poor oral hygiene may increase the risk of Alzheimer’s and dementia. Chronic inflammation and bacteria in the mouth may cross the blood-brain barrier, contributing to cognitive decline.
Protecting oral health may also help protect your memory.
Dental Tips for Seniors with Disabilities
Older adults with disabilities or dementia may struggle with brushing and flossing. Here are a few tips:
- Use electric toothbrushes with larger grips
- Create visual guides or checklists
- Use floss holders or interdental picks
- Consider professional in-home dental care services
- Schedule regular dental cleanings for seniors
Caregiver support is key in maintaining oral hygiene for elderly people with limited independence.
Final Thoughts: Prioritising Oral Health in Older Age
Good dental care for seniors is about more than teeth—it's about dignity, confidence, and better health. Whether you live independently or with assistance, make oral hygiene a daily priority.
If you haven’t had a dental check-up in a while or you're unsure where to start, reach out to your dentist or ask your local Just Better Care office for recommendations of a local dentist or if you have concerns about your oral health.
-(1).jpg?width=1500&height=1000&ext=.jpg&auto=format)



